I drove to the hospital today to do my follow-up bloodwork and to have post-op consultations with the surgeon and psychologist.
The transplant program psychologist was ready when I got there, so I actually met with her first. Just a brief chat about how I felt about the surgery and the recovery so far. She asked if there was anything I wish they had told me that they didn't, and the only suggestion I had was to remind donors of the potential for transplant cancellation or postponement. It never even crossed my mind that we might be cancelled, until it happened, and I think that's important for donors to be aware of. Otherwise, I felt well-informed.
I had my blood pressure taken right after that, and it was high, so the nurse took it again later (with a manual cuff the second time), and it was back to normal. Blood work, urine sample.
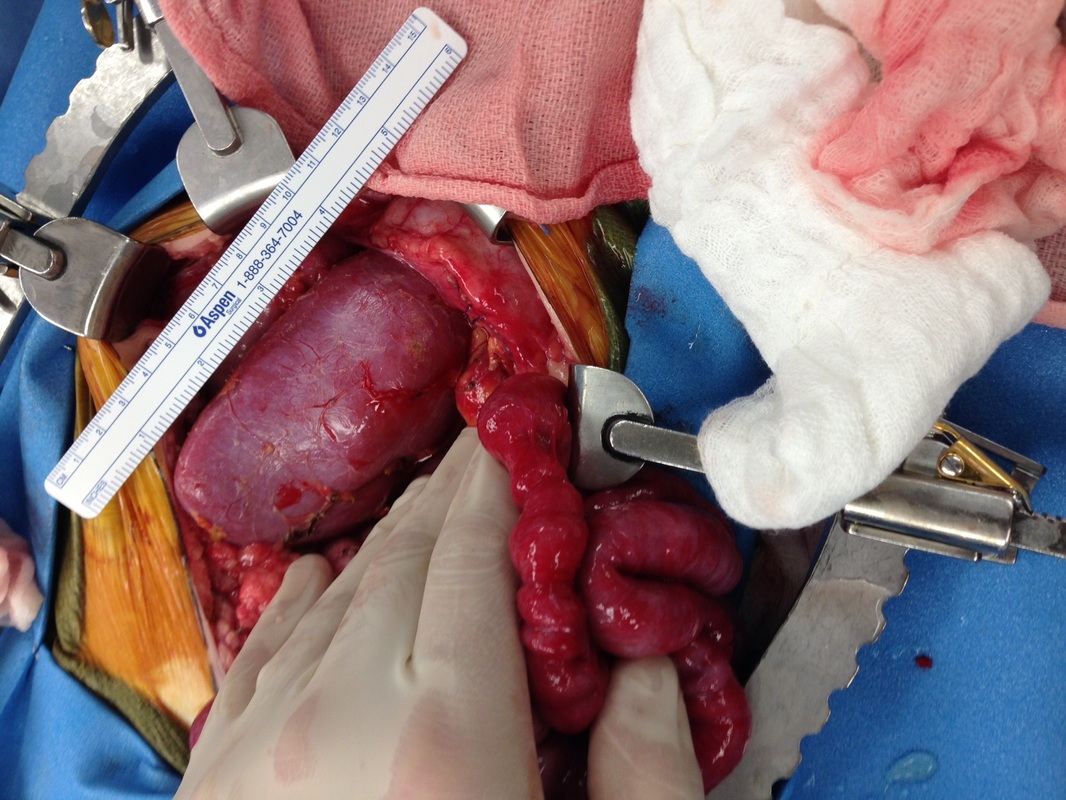
Then I met with my coordinator and a PA that I hadn't met before - I'm still not sure if he was around for the surgery and I just never met him, or if he wasn't even a part of the surgery. He checked my incisions, then consulted with the surgeon, who then came in to meet with me and check my incisions himself. Not really sure what the point of having the PA do it first was...
A couple stitches from under the skin had popped through, but will disintegrate, so the doc just snipped the one that was really sticking out. He said the incisions were looking great.
So then I started asking all my recovery questions - what specifically can and can't I do? He recommends a 5-pound restriction for the first six weeks, the other surgeons say 10 pounds. Yes, this includes body-weight exercises, like pushups and pullups (which I assumed, but thought I'd ask anyway).
Then they weightlifting conversation began. "Why do you lift weights?"
Uh...what? Because it's good for me. He apparently doesn't think weight lifting is a healthy activity. Whatever.
I asked if after the 6 weeks, I can start easing my way back into lifting weights or if I should wait longer.
He asked me how much I lift, the PA (who seems much more supportive of strength training) asks, "Are you squatting, like, 130 pounds?"
Yes, or more. Cleaning 100 or more. Deadlifting 200 or more. (Ok, my MAX is over 100/200. Not my regular weight.) :)
"Oh. Well....you don't want to lift that heavy for awhile. If you're dead lifting 200 pounds, you're really putting a lot of stress on that abdominal incision."
The surgeon butts in, apparently hasn't been listening to our conversation before that, "Can you lift that much?"
Well, two weeks ago I could.
"Oh."
Anyway, more questions, more explaining, he lets me know that at 6 weeks post-op I'll have about 70-80% of my abdominal strength back, but it takes at least 6 months for it to get to 100%, so it's risky to lift too much before then. After 6 months, "whatever happens is going to happen." (Which I took to mean, "If you hurt yourself after 6 months, it's because weight lifting is bad for you and you would have hurt yourself anyway.")
I asked a lot of questions, not to be annoying or because I want to push my luck on anything, but so that I can understand exactly how my body will be healing so that I can create a plan. If it takes me a year or more to get back to where I was two weeks ago, that's fine.
Asked about my kidney function and creatinine levels. He said that all my levels were what they expected, and my coordinator said it seems to take about a year for everything to get to where it'll be long-term. (Specifics about my levels below.)
I forgot to ask him about the nerve damage causing the 'sunburn' feeling on my left thigh. But, the area affected seems to be decreasing already, and my chiro said it can take up to twelve weeks to completely go away.
I talked to my coordinator about getting all my lab reports and records from my hospital stay. They have a great online chart system, but none of my inpatient info had been posted. I brought a form requesting records, and she said she'd make sure the records office got it. I asked her to make sure I got EVERYTHING, including any surgery notes, nurse's notes, etc. Although I don't know a lot of the medical terminology, I think it's interesting to read and I want to learn about exactly how my surgery went, etc. So hopefully they actually send it all to me.
Every six months for the next two years, I will get a letter/call from my coordinator reminding me to either visit her at the hospital, or see my primary care provider to get weight, blood pressure, urinalysis, and blood work. The information is kept for the hospital's own statistics, and is also sent to the United Network for Organ Sharing.
So, now for my kidney function levels:
The main blood tests referred to for kidney function are creatinine, BUN, and GFR. Donors should expect their levels to vary after surgery, as the remaining kidney will 'beef up' to take on about 30-50% of the lost kidney function.
BUN: Normal is 7-20. 2/12 (my initial testing) I was at 10, 7/18 (day of surgery) I was at 16, 7/19 I was 16. They either didn't test it today (7/30) or I just can't find it in the lab report. So I've remained normal there.
Creatinine: Normal for adult females is less than 1.2, although more muscle mass may make it a bit higher. 2/12: .8, 7/18: .9, 7/19: 1.3, 7/30: 1.1. So I'm already back to 'normal' for that.
Estimated GFR: This is essential the percentage of kidney function one has. Normal is 90+, but it's only worrisome below 60. Again, body type plays a role in the numbers. 2/12: 85, 7/18: 74, 7/19: 48, 7/30: 59.
These are the numbers I'll have checked every six months for two years, then yearly. I will never have 85+ GFR again, unless Righty is a super kidney and grows like crazy. But if I stay below 60 (which I doubt I will, since I'm already up to 59), or if my creatinine rises, it's not an automatic sign of an ill kidney. It just means I have one that cannot do the job of two.
After my appointments I stopped in to see Teddy and his mom. He's had some bumps in the road but Sarah says that overall he's doing well. He was talking and singing and dancing and playing the gravity game ("What happens when I drop this over the side of the crib? OH! Mama picks it up and gives it back to me!") Catch up with him at Sarah's blog.
The transplant program psychologist was ready when I got there, so I actually met with her first. Just a brief chat about how I felt about the surgery and the recovery so far. She asked if there was anything I wish they had told me that they didn't, and the only suggestion I had was to remind donors of the potential for transplant cancellation or postponement. It never even crossed my mind that we might be cancelled, until it happened, and I think that's important for donors to be aware of. Otherwise, I felt well-informed.
I had my blood pressure taken right after that, and it was high, so the nurse took it again later (with a manual cuff the second time), and it was back to normal. Blood work, urine sample.
Then I met with my coordinator and a PA that I hadn't met before - I'm still not sure if he was around for the surgery and I just never met him, or if he wasn't even a part of the surgery. He checked my incisions, then consulted with the surgeon, who then came in to meet with me and check my incisions himself. Not really sure what the point of having the PA do it first was...
A couple stitches from under the skin had popped through, but will disintegrate, so the doc just snipped the one that was really sticking out. He said the incisions were looking great.
So then I started asking all my recovery questions - what specifically can and can't I do? He recommends a 5-pound restriction for the first six weeks, the other surgeons say 10 pounds. Yes, this includes body-weight exercises, like pushups and pullups (which I assumed, but thought I'd ask anyway).
Then they weightlifting conversation began. "Why do you lift weights?"
Uh...what? Because it's good for me. He apparently doesn't think weight lifting is a healthy activity. Whatever.
I asked if after the 6 weeks, I can start easing my way back into lifting weights or if I should wait longer.
He asked me how much I lift, the PA (who seems much more supportive of strength training) asks, "Are you squatting, like, 130 pounds?"
Yes, or more. Cleaning 100 or more. Deadlifting 200 or more. (Ok, my MAX is over 100/200. Not my regular weight.) :)
"Oh. Well....you don't want to lift that heavy for awhile. If you're dead lifting 200 pounds, you're really putting a lot of stress on that abdominal incision."
The surgeon butts in, apparently hasn't been listening to our conversation before that, "Can you lift that much?"
Well, two weeks ago I could.
"Oh."
Anyway, more questions, more explaining, he lets me know that at 6 weeks post-op I'll have about 70-80% of my abdominal strength back, but it takes at least 6 months for it to get to 100%, so it's risky to lift too much before then. After 6 months, "whatever happens is going to happen." (Which I took to mean, "If you hurt yourself after 6 months, it's because weight lifting is bad for you and you would have hurt yourself anyway.")
I asked a lot of questions, not to be annoying or because I want to push my luck on anything, but so that I can understand exactly how my body will be healing so that I can create a plan. If it takes me a year or more to get back to where I was two weeks ago, that's fine.
Asked about my kidney function and creatinine levels. He said that all my levels were what they expected, and my coordinator said it seems to take about a year for everything to get to where it'll be long-term. (Specifics about my levels below.)
I forgot to ask him about the nerve damage causing the 'sunburn' feeling on my left thigh. But, the area affected seems to be decreasing already, and my chiro said it can take up to twelve weeks to completely go away.
I talked to my coordinator about getting all my lab reports and records from my hospital stay. They have a great online chart system, but none of my inpatient info had been posted. I brought a form requesting records, and she said she'd make sure the records office got it. I asked her to make sure I got EVERYTHING, including any surgery notes, nurse's notes, etc. Although I don't know a lot of the medical terminology, I think it's interesting to read and I want to learn about exactly how my surgery went, etc. So hopefully they actually send it all to me.
Every six months for the next two years, I will get a letter/call from my coordinator reminding me to either visit her at the hospital, or see my primary care provider to get weight, blood pressure, urinalysis, and blood work. The information is kept for the hospital's own statistics, and is also sent to the United Network for Organ Sharing.
So, now for my kidney function levels:
The main blood tests referred to for kidney function are creatinine, BUN, and GFR. Donors should expect their levels to vary after surgery, as the remaining kidney will 'beef up' to take on about 30-50% of the lost kidney function.
BUN: Normal is 7-20. 2/12 (my initial testing) I was at 10, 7/18 (day of surgery) I was at 16, 7/19 I was 16. They either didn't test it today (7/30) or I just can't find it in the lab report. So I've remained normal there.
Creatinine: Normal for adult females is less than 1.2, although more muscle mass may make it a bit higher. 2/12: .8, 7/18: .9, 7/19: 1.3, 7/30: 1.1. So I'm already back to 'normal' for that.
Estimated GFR: This is essential the percentage of kidney function one has. Normal is 90+, but it's only worrisome below 60. Again, body type plays a role in the numbers. 2/12: 85, 7/18: 74, 7/19: 48, 7/30: 59.
These are the numbers I'll have checked every six months for two years, then yearly. I will never have 85+ GFR again, unless Righty is a super kidney and grows like crazy. But if I stay below 60 (which I doubt I will, since I'm already up to 59), or if my creatinine rises, it's not an automatic sign of an ill kidney. It just means I have one that cannot do the job of two.
After my appointments I stopped in to see Teddy and his mom. He's had some bumps in the road but Sarah says that overall he's doing well. He was talking and singing and dancing and playing the gravity game ("What happens when I drop this over the side of the crib? OH! Mama picks it up and gives it back to me!") Catch up with him at Sarah's blog.






 RSS Feed
RSS Feed